When the National Institutes of Health launched the All of Us Research Program, the idea was simple: collect DNA and health data from over a million Americans to better understand how genetic variation influences health. But a newly published analysis of over 230,000 of these genomes has laid bare just how much complexity lies behind the terms "race" and "ethnicity"—and how that complexity can shape everything from disease risk to the ethics of medical research.
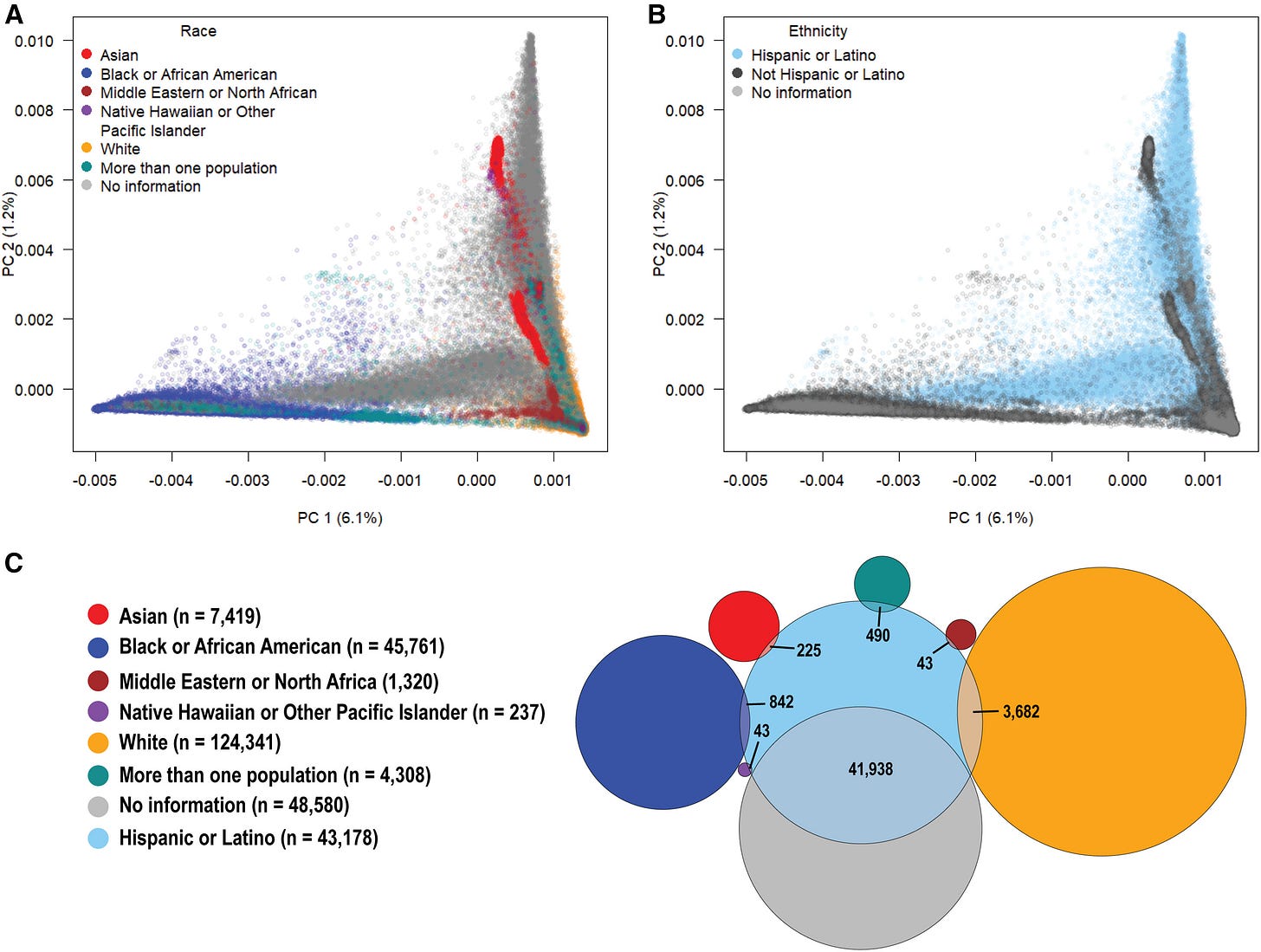
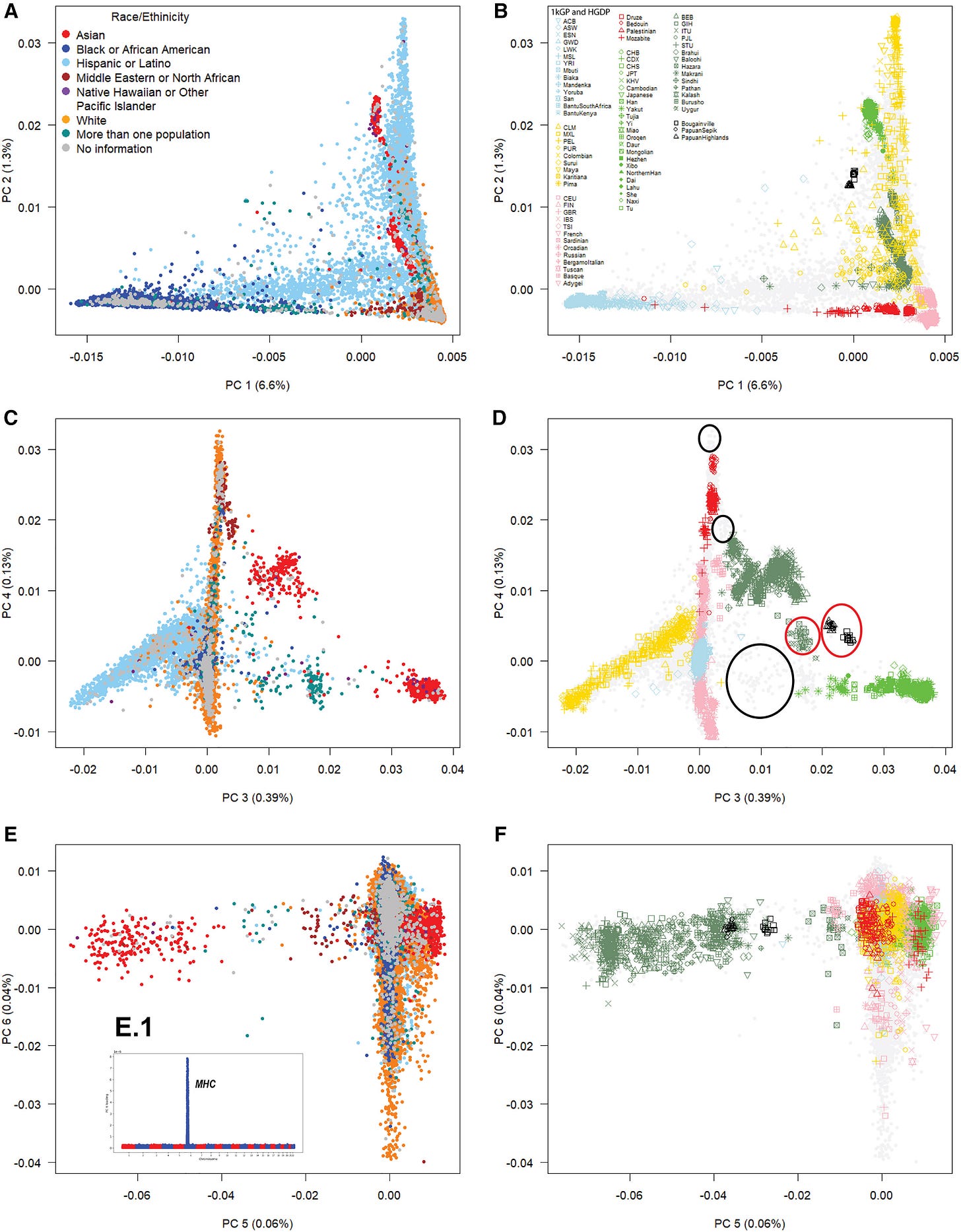
Drawing from nearly two million common genetic variants across the genome, researchers assembled what may be the most detailed map to date of the ancestry landscape in the United States. What emerged was not a set of neat, color-coded boxes, but a swirling, overlapping patchwork of human variation. For geneticists, this may not be news. For medicine and policy, it's a wake-up call.
"Participants within self-identified race and ethnicity groups exhibit gradients of genetic variation rather than discrete clusters."
That was one of the key findings of Mateus Gouveia and colleagues, who published their results in The American Journal of Human Genetics1.
The Limits of Labels
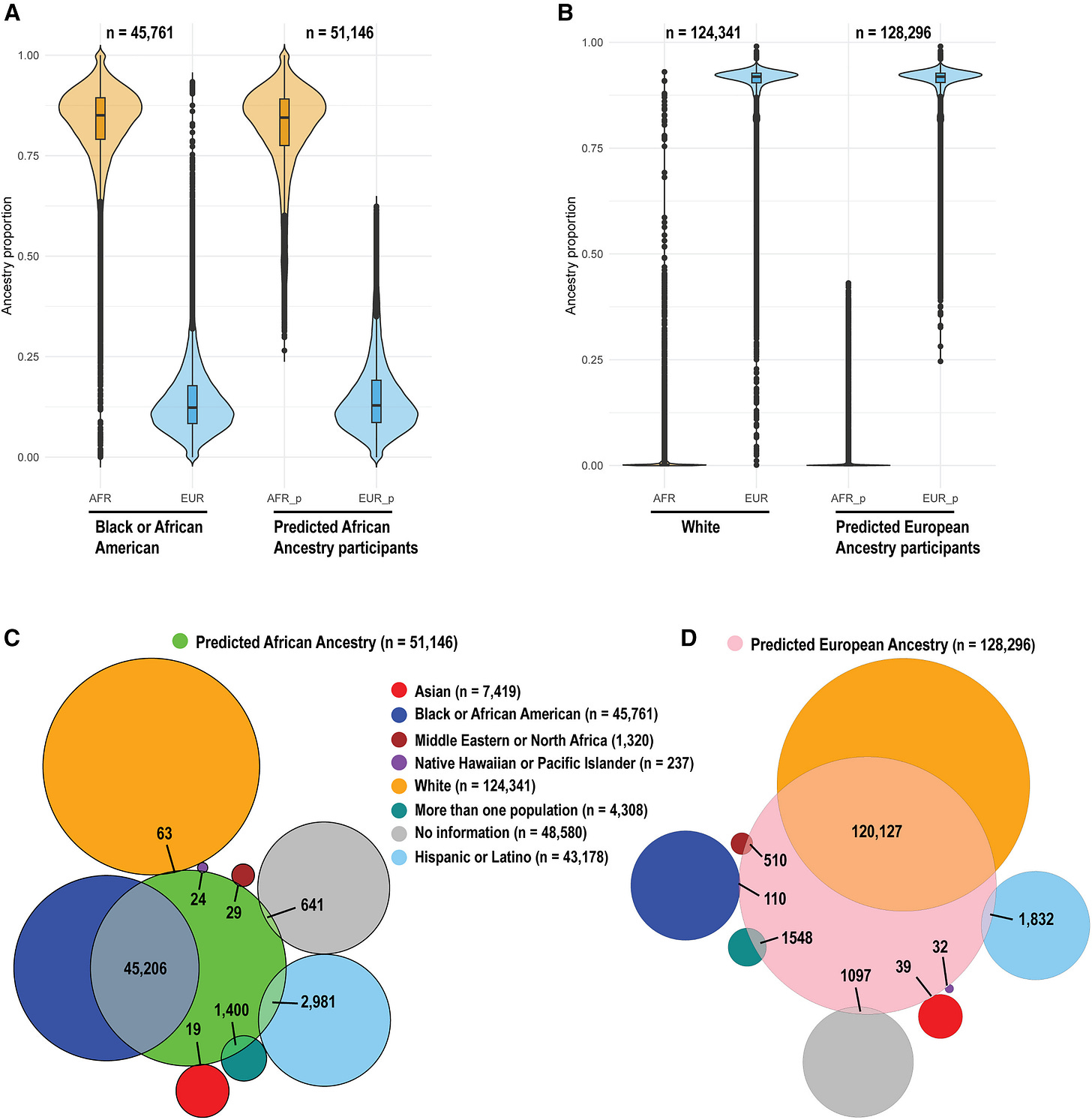
Most biomedical studies in the U.S. still rely on the racial and ethnic categories used by the Census Bureau: Black, White, Asian, Hispanic, and so on. But these social identities, while meaningful, fail to capture the biological histories embedded in our genomes. The All of Us data show that self-identification and genetic ancestry often diverge in important ways. For example, over 90% of participants who declined to self-report a racial category still identified as Hispanic or Latino. Their genomes revealed rich mixtures of African, Native American, and European ancestries, defying neat classification.
"Racial and ethnic categories are poor proxies for genetic ancestry."
The mismatch is not just academic. Genome-wide association studies (GWAS) that try to link genetic variants to disease often adjust for ancestry using race as a stand-in. That shortcut introduces bias. When subcontinental ancestries—like West-Central African versus East African—have different effects on health traits, lumping them into a single "African" category can obscure the biological signal.
Ancestry in the Body
To test the real-world effects of these ancestry distinctions, the team looked at two traits: height and body mass index (BMI). North European ancestry, for example, was strongly associated with taller stature. But within continental Africa, the results were more nuanced. West-Central African ancestry correlated with higher BMI, while East African ancestry correlated with lower BMI—differences that persisted even after adjusting for income, education, ZIP code, and other socio-environmental variables.
"Subcontinental ancestries can have opposite effects on biological traits and diseases."
This pattern appeared repeatedly across the dataset. Native American ancestry was associated with shorter stature and higher BMI, even when individuals self-identified as White or Hispanic. These associations hint at deeper population histories and may reflect ancient adaptations, demographic bottlenecks, or simply the layered complexities of gene-environment interaction.
The Geography of Admixture
The United States, with its history of colonization, slavery, and immigration, contains a striking range of human genetic variation. The All of Us data confirm this. African American participants in South Carolina, for example, showed elevated West African ancestry—reflecting known slave trade patterns and rice plantation histories. In contrast, Hispanic and Latino participants in New York showed higher African ancestry, likely due to Caribbean migration.
Even among White participants, subcontinental ancestries varied regionally. Northern European ancestry dominated the Midwest; Southern European ancestry was more common in the South. In New York and New Jersey, a noticeable slice of Middle Eastern ancestry stood out.
Implications for Medicine and Research
This mosaic of ancestries carries direct implications for medicine. Genetic risk scores for diseases like diabetes or hypertension may work well for Northern Europeans but perform poorly for people with mixed ancestries. Without fine-scale ancestry analysis, precision medicine risks becoming precision medicine for some.
The study also reinforces the value of moving away from monolithic categories. Instead of relying on broad racial labels, researchers are urged to adjust for detailed ancestry proportions—ideally down to the subcontinental level.
"We recommend treating continental ancestry not as a singular entity but as a composite of subcontinental ancestries."
That shift won’t be easy. Race and ethnicity are still used in health policy and public health surveillance. But the All of Us data show that when it comes to genetics, these categories blur more than they clarify.
What Comes Next
The All of Us database is still growing, and future studies will likely explore even finer-scale population structures. Already, researchers are planning admixture mapping studies to trace how specific gene variants inherited from different ancestries influence health. The ultimate goal is not just to improve medical care, but to understand how a nation's tangled genetic history shapes its present.
And that history, as it turns out, is more tangled—and more illuminating—than any census box can contain.
Related Research
Bryc, K., et al. (2015). "The genetic ancestry of African Americans, Latinos, and European Americans across the United States." Am J Hum Genet, 96(1), 37-53. https://doi.org/10.1016/j.ajhg.2014.11.010
Tishkoff, S. A., et al. (2009). "The genetic structure and history of Africans and African Americans." Science, 324(5930), 1035-1044. https://doi.org/10.1126/science.1172257
Lewis, A. C. F., & Green, R. C. (2022). "Precision medicine, but for whom?" Science, 375(6585), 589–591. https://doi.org/10.1126/science.abo0088
Mathieson, I., et al. (2018). "The genomic history of southeastern Europe." Nature, 555(7695), 197-203. https://doi.org/10.1038/nature25778
Gouveia, M. H., Meeks, K. A. C., Borda, V., Leal, T. P., Kehdy, F. S. G., Mogire, R., Doumatey, A. P., Tarazona-Santos, E., Kittles, R. A., Mata, I. F., O’Connor, T. D., Adeyemo, A. A., Shriner, D., & Rotimi, C. N. (2025). Subcontinental genetic variation in the All of Us Research Program: Implications for biomedical research. The American Journal of Human Genetics, 112(6), 1286–1301. https://doi.org/10.1016/j.ajhg.2025.04.012